Tracking patients’ health related quality of life alongside other aspects of their experience can help the NHS to improve services, says Tim Benson
Patients predominately want the health and care services to help them: avoid premature death; enjoy the best possible quality of life; to feel well physically and emotionally, be able and independent; and have a positive and safe experience of care that one would recommend to friends and family, with staff that treat you with compassion listen and communicate well, and prompt well organised services.
These aspirations are universal, irrespective of conditions comorbidities or types of treatment. They provide a solid starting point for the development of generic patient-centric quality measures.
‘The NHS has made remarkable progress during the past year in measuring how satisfied we are with the service we get’
Jim Collins, in Good to Great and the Social Sectors, stresses the need to use key performance indicators that are fit for purpose: “What matters is not finding the perfect indicator, but settling upon a consistent and intelligent method of assessing your outcome results and then tracking your trajectory with rigour.”
How is the NHS doing?
Survival: We have made good progress on survival. We record deaths and their causes. Life expectancy has grown substantially. Domain 1 of the NHS outcomes framework aims to prevent people from dying prematurely and overarching measures are in place. Following the Francis and Keogh reports, the role and uses of standardised mortality rates have become clearer.
However, mortality is a lagging indicator, is rare for many services and needs substantial adjustment for risk. There are limits to what it can say about how things are right now.
Quality of life: After survival the most important thing is how we feel and how much we can do − health related quality of life (HRQoL). This relates closely to domains 2 and 3 in the outcomes framework. Yet the NHS has made little progress in collecting patient’s own perception of their HRQoL as part of day to day care processes although this should be part of each patient’s history.
Specialist clinical communities and pharmaceutical companies dominate research on HRQoL measures and have developed innumerable condition specific measures for use in clinical trials. Far less effort has been devoted to generic measures.
More than 40 years ago Rosser and Watts’ seminal paper, The measurement of hospital output, described the use of a simple generic measure across a 300 bed general hospital. They measured each patient’s HRQoL on admission, on discharge and at follow-up for one month. No one has repeated this since.
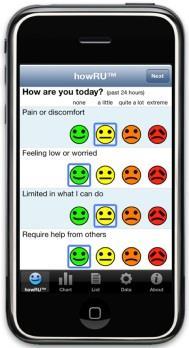
In 1976 I became Rosser’s PhD student and have sought to continue her work with howRU, an ultra-short generic HRQoL measure. The results for patients with long term conditions are at least as good as alternatives that are far more burdensome. The howRU Health Tracker is designed for repeated use on a smart phone or tablet and has been available on the iPhone App Store since August 2010.
Experience of care
The NHS has made remarkable progress during the past year in measuring how satisfied we are with the service we get. The friends and family test has been implemented across all inpatients, accident and emergency and maternity care. Plans are being put in place to extend it to most other health, social care and public services within the next 18 months. This demonstrates that given political will, new measures can be implemented rapidly successfully and at scale.
On its own the test can identify that a problem exists but is silent about the cause. For this reason the test requires follow-up questions, which may be free text, structured or both.
‘People have begun to understand that what really matters is how we use information to improve services’
When we use tools like TripAdvisor to choose a restaurant we look not only at the overall rating score but also at the sub-scales for value, service, atmosphere and food, as well as comments. In a similar way we have developed additional questions known as howRwe, covering compassion (treat me kindly), communication (listen and explain), promptness (see me promptly) and organisation (well organised). These look and feel similar to howRU and add richness to friends and family test data.
Routine use of mortality and friends and family data shows what can be done. People have begun to understand that what really matters is how we use information to improve services. This would be much easier if we also tracked HRQoL and other aspects of patient experience.
Tim Benson is founder of Routine Health Outcomes, @timbenson



























No comments yet