There is an urgent need to reform the system for paying and contracting for services in the NHS but new complex financial incentive schemes are not the answer, writes Ben Collins
Over the last 30 years, the English NHS has repeated a peculiar managerial ritual: the development of payments, incentives and contracts to reward health services for performance. Despite the disappointments, national policymakers have remained convinced that their latest round of payment reform would finally create a self-improving health system.
Each iteration of the ritual has ended in failure. Devised to increase activity, the national tariff has continued to focus resources on hospital services when they need to be moved into primary and community care.
Our current combination of piecework payments for hospitals and capitation or block contracts for primary and community care incentivises the wrong things in the wrong places.
Meanwhile, there is little evidence that incentive schemes such as Commissioning for Quality and Innovation have delivered substantial improvements in quality or efficiency.
New incentive schemes
Nevertheless, the enthusiasm for complex new incentive schemes remains unabated.
Under the most recent proposals for integrated care, NHS commissioners are being encouraged to bring together new “whole population annual payments” and contract with a single integrated care provider or partnership to deliver services for a local population, with new incentive payments to motivate performance and renewed efforts to transfer risk and reward to providers of services.
At the heart of these schemes, there is an enduring conviction that recalibrating financial incentives will have a predictable, mechanical effect on a complex system.
In this clockwork universe, smart technocrats just need to pull the right levers and put in place appropriate supporting conditions to trigger improvements in health services’ performance. This despite an ever-growing body of evidence that financial incentive schemes routinely have perverse consequences.
While English policy makers have been gazing over the Atlantic, other countries with tax-funded health systems have been heading in an entirely different direction
Our new paper, Payments and contracting for integrated care, questions whether these latest payment schemes will be any more successful than their predecessors. The architects of new payments and contracting models for the NHS appear to have been heavily influenced by accountable care in the US, despite the differences between tax-funded and insurance-based health systems.
Indeed, how to apply financial incentives to useful effect in public health systems is an enduring challenge. If the state withholds payments from underperforming providers, this simply makes it harder for them to deliver adequate services: the absurdity of punishing patients who have already been let down by risking even worse care. In practice, the state often bails out failing providers, undoing the effects of the scheme.
Economists have highlighted the transaction costs of attempting to make these incentive schemes work. When commissioners seek to harness financial incentives, it becomes important to pin down the circumstances in which payments should be made or withheld.
When they seek to transfer risk and reward, they must develop contracts that prevent providers escaping those risks if they transpire, for example cutting their losses by terminating the contract early. They need to specify how the parties will deal with changing circumstances, for fear that they will use changes as an excuse for reneging on commitments or renegotiating the deal.
In short, they find themselves attempting to write complete contracts that cover every eventuality, a costly and ultimately futile endeavour for complex groups of services over long contracting periods.
While economists might calculate the considerable transaction costs, it is hard to put a figure on the wider consequences, for example, the local leaders locked in recriminations about targets and payments rather than developing more constructive, collaborative approaches to the stewardship of local systems.
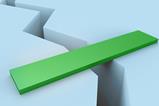
There is an alternative way forward. While English policy makers have been gazing over the Atlantic, other countries with tax-funded health systems have been heading in an entirely different direction.
In New Zealand, the Canterbury Health Board abandoned transactional approaches to managing its local health system in the late 2000s.
Rather than complex incentive schemes, it focused on developing with providers a compelling vision for services and the management systems needed to improve performance. Rather than attempting to transfer risk and reward to providers, it recognises the state’s responsibility to run a stable public health system.
Rather than algorithms to apportion gains or losses, it agrees with providers how to reallocate resources to meet the community’s needs.
There is an urgent need to reform the system for paying and contracting for services in the English NHS. But new complex financial incentive schemes are not the answer.
Across England, commissioners and providers in local systems – Bolton, South Tyneside, Leeds and many others – are abandoning arm’s length contracting in favour of collaborative relationships.
In 2016, the clinical commissioning group and acute hospital in Bolton agreed to put aside transactional approaches and work together in the interests of the local system. They replaced payment for activity with block contracts and simple arrangements for sharing costs or savings.
These new arrangements are still evolving, but they are already delivering benefits. Both commissioner and provider have achieved substantial savings and staff who used to work on disputes are now collaborating on improvement.
If such transformation is possible, it may be because these new ways of working are not entirely new. They reconnect with traditions of collaboration in public services that have been obscured temporarily but remain core to the NHS.






























4 Readers' comments