High costs, complex planning and ‘pilot-itis’ are all common hurdles to technology adoption. Sally Chisholm argues a coordinated national approach could help overcome them.
Traditionally, adopting new technologies and procedures – as well as measuring their subsequent success – becomes more complex the larger the organisation. But it does not have to be this way.
At the moment, adoption of innovative technologies happens because of individual people or individual NHS organisations at local or regional level. They take it on themselves to try to create a culture or to use innovation funds to engage people. This is great but it is not the same as having a robust, systematic approach across the NHS.
It is widely recognised that there needs to be a function that supports people in this. People who work in frontline NHS services are very busy and often they do not have the expertise or time to research, test and measure the success of new technologies – hence the lack of a “pull culture”.
The NHS Technology Adoption Centre was launched in 2007 and its original brief was to understand the barriers to technologies entering the NHS. We have developed specific knowledge about how to overcome them.
Top tips for adopting innovation
There are two fundamental questions which need to be considered before implementing healthcare technologies into the NHS:
- Is the technology ready for market, and can it demonstrate its benefits?
- Is there an unmet need that will create a demand for it?
If the answer to both of these questions is yes, then the challenges which follow involve:
- generating commitment from across all of the departments/organisations that the technology will affect or influence (this is likely to be far wider than first considered);
- gathering the data which will provide, beyond doubt, that the technology offers patient benefit and is cost effective when used in routine clinical care;
- identifying the changes needed for sustainable adoption – revised clinical pathways, robust procurement, staff training, effective communication and decommissioning “redundant” aspects of care for example.
These tasks may sound simple but in order to be achieved require a clear understanding of the bigger picture as well as the workings of the wider NHS. This means investing time in understanding how changes could, or will, affect others, most importantly of course the patients receiving care.
By applying a methodical approach and providing all of the tools and resources necessary the NHS Technology Adoption Centre offers trusts access to “implementation expertise” which supports successful and effective adoption of healthcare technologies.
Our approach has involved supporting practical adoption on the NHS front line of proven technologies that represented a major, step-change innovation; had a serious adoption issue (that is, had clearly demonstrated improved outcomes or efficiencies but had minimal take-up); supported a clinical area of major focus in the NHS; and supported national policy priorities.
Adoption of technology can be very complex. New methods can mean new training, while care pathways often have to be redesigned, meaning potentially disruptive staffing and organisational changes. Also, existing procedures have to be decommissioned.
Let’s say you needed procedure A, B and C in a particular care pathway but, by adding D, you don’t need A and B anymore. But if A and B are not decommissioned then you end with four procedures – duplication and extra costs rather than savings.
Financial barriers to innovation represent another hurdle. New technologies may offer proven long term benefits but a particular department or organisation may be dissuaded from implementing them if a new procedure costs more than its predecessor. This could be dealt with by a mechanism introducing a temporary national tariff to cater quickly for innovation-related improvements.
Similarly, one department may find itself facing an increased cost if it embraces an innovation while the saving will go to another department further down the care pathway or indeed another NHS organisation.
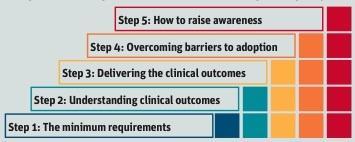
Adoption Roadmap
The NHS Technology Adoption Centre has developed a generic adoption process to offer a systematic and robust methodology “road map” to organisations looking to introduce new technologies. One of its strengths is that the centre developed this through its work with the NHS, industry and patient groups. Crucially, the process does not just involve the management of change but also includes ways of collecting data, according to pre-established metrics, to accurately measure the impact of that change.
Once the NHS as a whole is able to accurately measure its success as an innovative organisation, then the Technology Adoption Centre will be better able to measure its influence as a catalyst in the drive for greater innovation, lower costs, better outcomes and greater quality.
And then there is “pilot-itis”. It is often the case in the NHS that we want to test every product ourselves before introducing it, either because we feel our health economy is different from everywhere else or simply because we did not develop it, even though it may have been widely used elsewhere with great success and have won NICE approval.
In our submission to the Department of Health’s innovation review we recommended that an NHS wide resource, with a coordinated, systematic approach to adopting, measuring its effectiveness and spreading innovation across the NHS, could have a vast effect on patient care, on costs and, indeed, on the economy as a whole. Not least because at present without such a function individual trusts and companies have to try and find their way through the highly complicated innovation landscape alone and without the benefit of access to expert support and advice.
Making the case
The How2Why2 guides are designed to illustrate to NHS management and clinicians how and why they should go about adopting certain selected new technologies.
The guides include relevant practical examples such as draft business cases, suggested revisions to care pathways and training requirements. The NHS Technology Adoption Centre’s case study on the use of insulin pump therapy has been reported by clinicians as “evidence of an official ‘steer’ towards better use of technological advances and a vote of confidence in its safety and efficacy”. Strikingly, though, many areas across the UK have a take-up of less than 1 per cent, compared with some countries where it is nearing 40 per cent.
We supported the adoption of oesophageal doppler, a technology which could pave the way to savings of £400m for the NHS each year as well as delivering reduced hospital stays and mortality.
Another How2Why2 guide, on the breast-lymph-node assay, tackles many of the potential barriers to adoption. The case study shows that this new intra-operative test – as opposed to the sentinel lymph node biopsy commonly used for the assessment of lymph-node spread in early breast cancer – would remove the need for a second surgical procedure for 11,000 patients each year. This is a significant quality gain. It would also save 24,000 bed days across the NHS, equating to a saving or efficiency gain of £4m a year on ward costs alone.























No comments yet