Cath Cooksey, NHS lead medicines optimisation pharmacist, Kent and Medway Integrated Care Board, describes educational initiatives to implement regional asthma guidelines.
Intended for HCPs and relevant healthcare decision makers
Sponsored by and written for
It is now more than 10 years ago that The National Review of Asthma Deaths reported on Why asthma still kills.1 While advances have been made in the decade since, more than 12,000 people have died from asthma2 and there remains a need for further improvements in care and more comprehensive adoption of the report’s recommendations.
Overuse of short-acting beta-2 agonist reliever inhalers adversely impacts asthma outcomes.3,4 There is compelling evidence that using anti-inflammatory reliever therapy and maintenance and reliever therapy reduces the risk of severe asthma attacks compared with SABA monotherapy.5 However, attitudes to the issue have been slow to change,5,6 with 1.9 million people in the UK still being prescribed three or more SABA reliever inhalers in 2023.7 Furthermore, SABA overuse is a significant contributor to the carbon footprint of respiratory treatment.8
Updating regional guidelines and building relationships
On starting my current role in 2021, it was clear that patients with asthma in Kent and Medway should be a priority. For example, hospital admissions for paediatric patients with asthma were well above the national average.
Owing to there being no up-to-date guidelines for England at that time, the Kent and Medway Integrated Care Board decided to develop new regional asthma guidelines in line with the Global Initiative for Asthma guidance.9 We sought to move towards the adoption of the AIR and MART approaches to asthma management to improve patient outcomes.
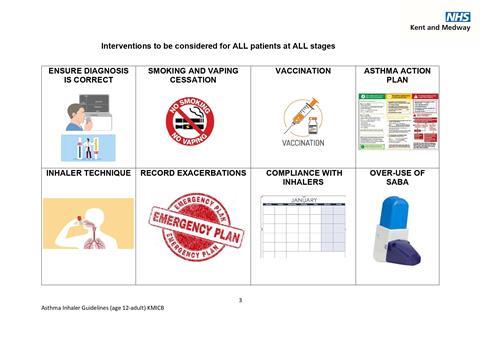
We worked in partnership with multidisciplinary healthcare stakeholders to deliver and implement regional guideline changes. These relationships enabled us to provide education, creating awareness of our guidelines and the rationale underpinning them.
Using educational campaigns to improve asthma outcomes
Primary care has always been central to guideline implementation and has become the focus of our regional educational campaign. The programme included a webinar series, face-to-face events, and ICB Respiratory Days. More than 400 healthcare professionals have participated, including from primary care, community pharmacies and two acute care trusts. Training was given to reception staff to help them in allaying patient concerns that may arise. Additionally, an asthma-friendly schools programme,10 which now has 32 local schools accredited, was initiated, funding was secured for a paediatric nurse to visit schools and offer support in GP surgeries, and substantial support was provided by the voluntary sector. Work to partner with local football and rugby clubs is now in progress.
Engagement was undertaken to demonstrate the feasibility of implementing the new guidelines, including in terms of budget and resource allocation.
Achievements, remaining challenges and new opportunities
Our educational campaign achieved a 49 per cent reduction in patients prescribed six or more SABA reliever inhalers in a year and a 67 per cent reduction in patients receiving two or more oral corticosteroids.
Regional and local initiatives focused on issues such as SABA overuse continue to rely on supportive messaging from the national level. This highlights the need for a national change in asthma management, and the publication of the new British Thoracic Society/Scottish Intercollegiate Guidelines Network/National Institute for Health and Care Excellence joint guideline11 is welcome.
The next important step for our programme is patient education and engagement to allow us to understand better, and challenge where appropriate, their perspectives and perceptions. A method to track inhaler use would be tremendously valuable in allowing us to assess the impacts of implementation programmes. A dashboard that allows us to see changes, in real-time, in the use of SABA, AIR and MART, in the context of GP appointments and hospitalisations would be ideal.
With the recent publication of the BTS/SIGN/NICE guideline, this is an ideal time to update guidelines and practice across the country, to address the key recommendations of NRAD and reduce morbidity and mortality in our asthma patients.
Job Number: GB-61122
Date of preparation: December 2024
References
1. The National Review of Asthma Deaths. https://www.rcp.ac.uk/media/i2jjkbmc/why-asthma-still-kills-full-report.pdf (accessed November 2024)
2. Asthma+Lung UK: ‘Asthma care is in crisis’ - charity sounds the siren as asthma death toll rises. https://www.asthmaandlung.org.uk/media/press-releases/asthma-care-crisis-charity-sounds-siren-asthma-death-toll-rises#:~:text=preventable%20asthma%20deaths-,Over%2012%2C000%20people%20in%20the%20UK%20have%20died%20from%20asthma,of%20asthma%20deaths%20are%20preventable (accessed November 2024)
3. Quint et al. J Allergy Clin Immunol Pract. 2022;10(9):2297–309.
4. Bateman et al. Eur Respir J. 2022;59(5):2101402.
5. Levy et al. Br J Gen Pract. 2024;74(739):86–9.
6. McKibben et al. NPJ Prim Care Respir Med. 2018;28(1):26.
7. AstraZeneca: 10 Years on from the National Review of Asthma Deaths. https://www.astrazeneca.co.uk/media/articles/review-of-asthma-deaths.html#accordion-3d089f749d-item-91de328b08 (accessed November 2024)
8. Wilkinson A, Woodcock A. Br J Clin Pharmacol. 2022;88(7):3016–22.
9. GINA reports. https://ginasthma.org/reports/ (accessed November 2024)
10. Transforming Partners in Health and Care: Asthma Friendly Schools https://www.transformationpartners.nhs.uk/resource/primary-care-children-young-peoples-toolkit/schools/asthma-friendly-schools/#:~:text=The%20asthma%20friendly%20schools%20programme%20sets%20out%20clear%2C,people%20with%20asthma%20at%20primary%20and%20secondary%20schools
11. Asthma: diagnosis, monitoring and chronic asthma management (BTS, NICE, SIGN) https://www.nice.org.uk/guidance/NG245



























