Pressure ulcers can be devastating for the patient but are finally being given a higher profile nationally, writes Jennifer Trueland

Ruth Ropper is passionate about preventing pressure ulcers and recognises the need to get managers on board. But rather than show them the figures, she says the surefire way to get managers to take pressure ulcers seriously is to show them the pictures.
“Images have a real impact,” she says. “People can really see for themselves what we’re talking about, and how horrible it is for patients. Patient stories help, too - hearing from the people the effect that pressure ulcers have on them, and on their families.”
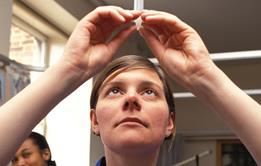
Ms Ropper, a member of the UK Tissue Viability Society and a tissue viability nurse specialist with NHS Lothian, explains what pressure ulcers mean to patients.
‘I don’t think we’ll ever get to zero pressure ulcers but we’re looking at what’s avoidable and what isn’t’
“If somebody develops a pressure ulcer it impacts their whole life,” she says. “If you’re unwell you take longer to heal, if you have an open wound you’re at risk of infection, you might have to have repeated dressings, it can affect your body image - the impact on the individual and the family is huge, which is why preventing it is very, very important.”
The figures are also eye watering. According to research published in the Journal of Wound Care last year, the costs of treating a pressure ulcer vary from £1,214 for category 1 (least serious) to £14,108 for the most serious category 4 ulcers.
The now defunct NHS Institute, which included pressure ulcers as one of its high impact actions, quoted research suggesting that pressure ulcers occur in between four and 10 per cent of patients admitted to hospital, and around 30 per cent of people in nursing homes.
Citing 2004 research, it estimated the cost to the NHS of treating all hospital acquired pressure ulcers as between £1.4-£2.1bn per year - to put that in context, that was around 2 per cent of the entire NHS budget when the research was conducted a decade ago.
Not the way to go
In the last few years, pressure ulcers have begun to receive high-level attention. Just last month NHS England published its business plan for the next three years. Among the measures to improve the patient experience is a commitment to rolling out public reporting of pressure ulcers.
Also at a national level, the National Institute for Health and Clinical Excellence is working on new guidance on pressure ulcer prevention, updating its 2005 guideline and the organisation has also published a pathway on pressure ulcer management.
In England, initiatives such as the Patient Safety Thermometer (which includes measurement of pressure ulcer prevalence) have been introduced, and there are commissioning for quality and innovation (CQUIN) payments tied to pressure ulcer measurement, in a bid to improve quality.
Not everybody agrees with this method, however. Although delighted to see pressure ulcers taking a higher profile, Alison Hopkins, outgoing chair of the Tissue Viability Society, and chief executive of Accelerate CIC, which provides specialist wound and lymphoedema services to the NHS, argues that prevalence measurement is not the way to go.
“The poorest wards will have the lowest prevalence because they won’t record them,” she says, adding that prevalence does not take into account things like case mix.
Grading ulcers at any one point in time is also problematic, she says, because sometimes it is not immediately clear. For example, someone with a black mark on their heel might simply have a blister with hard skin that will fall off, or they could have deeper damage which, in a diabetic, might mean losing a leg. “We don’t know what it is until we’ve watched and waited,” she says.
The SSKIn tool
Of course it is important to pick up where negligence has been a contributor, but classification of an ulcer as a 3, for example, does not necessarily imply negligence.
There are a number of toolkits and initiatives designed to prevent pressure ulcers. The NHS Institute Skin Matters work (still available on its archive website) includes case studies of how trusts and others went about trying to tackle the issue and reduce the harm - and the bill.
In Scotland, health boards are encouraged to use the US-developed SSKIN tool, which asks nurses to consider: Surfaces, such as mattresses and cushioning; Skin inspection; Keep moving; Incontinence (including moisture); and Nutrition. Money has been allocated to boards to promote pressure ulcer prevention, although it is up to each board to decide how to use it.
At NHS Lothian, Ms Ropper has been funded to run a year-long programme supporting pressure ulcer prevention. The “One a Day to None a Day” initiative was so named because data suggested that Lothian hospitals had around 32 pressure ulcers per month - almost one a day - and the idea was to reach zero.
The project involves link nurses, who are educated and supported to raise awareness in their clinical areas, as well as the development and distribution of resource packs. Around six months into the project, numbers of pressure ulcers have almost halved - there were 17 in March - but it is anticipated that raising awareness will push the numbers up in the short term.
“I don’t think we’ll ever get to zero pressure ulcers, but we’re looking at what’s avoidable and what isn’t,” says Ms Ropper.
Board support
Ms Hopkins believes that the big change that is needed is cultural - pressure ulcers have to be seen to be the business of everyone in the multidisciplinary team.
“The doctors who clerk the patient in should be looking at the skin, the physio should be looking at the skin. At the moment we have people in silos - skin is ‘nurse’, ankle rotation is ‘physio’ and medication is ‘doctor’,” she says.
High-level board engagement and senior management engagement is also essential as this determines funding decisions. “Yes, you have to get support at board level,” says Ms Hopkins. “But they have to really understand the statistics - otherwise it makes a mockery of what we’re doing and becomes a way of bashing nursing staff.”
And that won’t help patients. “Pressure ulcers are a hugely important issue,” she says. “And I’m glad they are being taken seriously, but we’ve got to get this right.”
Paul Trueman on a major indicator of care quality
When the National Quality Forum in the United States deemed pressure ulcers to be “never events” it prompted a debate about the degree to which pressure ulcers can be classified as avoidable or non-avoidable. Whatever your view, such bold statements have changed the way pressure ulcers are perceived. Most in the NHS now view healthcare acquired pressure ulcers as a patient safety concern on a par with medication or surgical errors.
From a patient’s perspective, pressure damage to the skin is traumatic and painful. They develop as a result of an individual receiving inadequate preventive care when they are immobile or incapacitated, for example, following spinal or trauma injuries. For these patients, the development of a pressure ulcer adds insult to injury.
Pressure ulcers are also costly to treat and it’s true to say that prevention is far cheaper than the cure. Yet the economic impact described in this supplement is poorly recognised by many in the health service - as is the ability to make massive changes for a small investment.
Experience in the US following the National Quality Forum’s declaration have shown us what can work. Policies that align funding to performance, to ensure that hospitals no longer receive funding for the management of patients who develop “never events”, can be a mechanism to change behaviours. Promoting pressure ulcer management as an indicator of care quality and sharing information on pressure ulcer incidence publicly can also have a powerful effect.
Here in the UK, it is vital that board level sponsorship is in place to raise awareness and drive behaviour change. Pressure ulcers should be regarded as an indicator of care quality that has the potential to impact on trust performance indicators and income, for example through CQUIN payments.
Policy initiatives such as the Safety Thermometer and the QIPP programme have helped to raise awareness at senior management levels. Reassuringly for boards, many of the initiatives that can reduce pressure ulcer incidence are relatively low cost.
Undoubtedly, initiatives to address pressure ulcers lack some of the “glamour” of other trust activities. However, their prevention is a fundamental part of ensuring high quality patient care, promoting patient safety and health service efficiency. On this basis they are deserving of more attention.
Paul Trueman is Smith and Nephew’s vice president of market access
Patient Safety − an HSJ supplement
From better workforce vetting to new approaches to tackling pressure sores, the latest thinking on patient safety
- 1
- 2
 Currently
reading
Currently
reading
Facing up to the painful truths about pressure ulcers
- 4
- 5
- 6
- 7




































No comments yet