The concept of a closed loop patient journey would enable the system to learn about the patient, so that each episode of care is more personalised to that patient, or to patients like them, writes Stuart Bailey
With the NHS facing an increasing challenge of responding to urgent and emergency care and “record waits for planned surgery and in accident and emergency, as staff plough through a backlog fuelled by covid” (NHS faces an Easter “as bad as any winter” - BBC News), is it time to re-imagine the way that patient journeys are managed, by turning the data that sits inside the wider system into information and actionable insights?
At the moment, unscheduled care is generally a reactive linear journey, with a patient using whatever means they can to access the NHS. This can range from visiting a pharmacy for advice, getting an appointment with their GP, ringing NHS 111, dialling 999 or heading to the nearest A&E.
Sponsored by
Patients are also using “Dr Google” or a variety of information, both good and less helpful, from the Internet – many charities have fantastic resources available that help with specific conditions or issues, but most of the general public are poorly equipped to separate the wheat from the chaff in the information that searches will return.
Each of these routes to access care or advice are delivering the best services they can with limited resources, and are all acting in the best interest of the patient, striving to provide the best outcome for that episode. Often, though, the service accessed is not the most appropriate for the situation that the patient is in, which either results in a large amount of effort helping the patient or delays due to referrals – or “the run-around” as many patients would refer to it.
The system is set up so that GPs receive notifications of many of the episodes of care that their registered patients receive, with NHS 111 or 999 Post Event Messages and letters from other services arriving through the digital channels that the last 10 years have established. General Practice, however, is under intense pressure, with doctors leaving the profession and “GPs seeing ‘almost double’ recommended numbers of patients” (“Uberisation” of general practice creates safety risk, warns Hunt | News | Health Service Journal (hsj.co.uk)). It faces huge workforce issues and workloads, and is also being impacted by conditions that have not been detected during the pandemic period and increasing instances of long covid. Whilst general practice still seeks to “know their patients”, and to be responsible for their care, it is increasingly likely that a holistic view of a patient is not maintained.
So, what does a linear, reactive, patient journey result in?
Given the same presenting issue, it’s likely that the same outcome will be reached each time, unless something else disturbs that process – as Einstein may or may not have said, “Insanity is doing the same thing over and over and expecting different results.” Each episode will follow a similar path, dependent on the service being used, but will look something like this sort of flow:
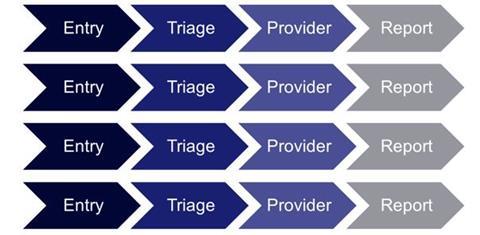
Thus, unless the system or the patient learns from previous encounters, the patient’s journey will be the same – and may result in an unfulfilled need. This is even more apparent when we look at services such as NHS 111, who, in general, simply direct a patient to the most appropriate service – they have no knowledge whether the patient actually did what was advised. And we know that patients often don’t do what they are told, not through a sense of entitlement, but more because what they are told doesn’t fit with their expectations.
This can lead to conditions being managed symptomatically and underlying issues going unnoticed and untreated, until the patient ends up with either a more significant symptom or with a service that investigates a more complete history.
So – what could be done differently?
It’s my view that the concept of a closed loop patient journey would enable the system to learn about the patient, so that each episode of care is more personalised to that patient, or to patients like them.
In this context, a closed loop journey means getting information from multiple interactions of the patient with services and “understanding” what that means for the patient. This could involve using ED records, pharmacy visits, GP visits, OOH records, social care records, as well as other risk-stratification measures.
This enables more “thought” to be put into the process of deciding what the patient’s journey should be at each entry point.
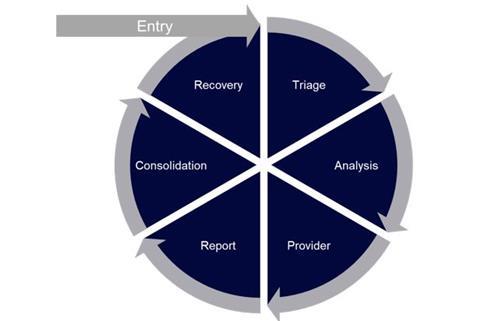
That “thought” could be as simple as referring them to a dedicated clinical team when triggers are found – who would take a more comprehensive view of the patient, with a history that starts to tell their story. That would, in turn, inform how that individual is cared for, looking at a patient longitudinally, rather than just episodically, and using personalised actionable insights to deliver better care and better outcomes.
That also enables more “thought” to be put into the process of managing cohorts of patients – looking at the whole cohort along a different axis (I’d say latitudinally, but that doesn’t really make sense!) Cohorts of similar patients can be identified where the same personalisation would be effective can be identified, in a similar way to how the vaccination programme, for example, has used cohorts to understand risks.
Could this be regarded as “risk stratification on steroids”, generating further actionable insights that can, for example, inform screening or other preventative measures? Would this start to solve some of the challenges we have with resourcing screening programmes across the NHS? Is the introduction of integrated care systems the time in which this sort of change can be instigated?
With the amount of data that is now captured through the various services used by patients, we must be able to turn some of it into information that can allow clinicians to drive the creating of these actionable insights – and then make use of these to reduce the burden on overstretched services.
I’d be really interested to hear the thoughts of others about how a closed loop system could drive better outcomes and experience for patients alongside reducing waste and improving efficiency within the health system as a whole.




























No comments yet