Understanding why patients do not adhere to treatment or make positive lifestyle changes is vital to improve outcomes, writes Alison Moore

Providing healthcare would be so much easier if the public always did what was asked of them. From changing lifestyles to taking medicines they are prescribed, there are numerous opportunities to help patients improve their outcomes.
But it is an imperfect world and patients sometimes do not do what is best for them. And that can lead to poorer outcomes and waste.
‘Patients sometimes do not do what is best for them’
Patients are often passive consumers of care rather than active participants in their own health management. Encouraging them to change could help the NHS plug the approaching crisis of an older population and increased prevalence of chronic conditions.
Don Redding, policy director of patient charity coalition National Voices, says adherence must always be seen in the context of how much patients are engaged in their own health and care.
The National Institute for Health and Care Excellence emphasises that adherence is often related to patient knowledge and confidence about taking medications, and there is evidence that patients involved in decisions about their own care are more likely to adhere to medicine or monitoring.
Helping patients make the right choices may not save money but it is likely to improve outcomes for the same money, Mr Redding says. Patients may opt for less intervention such as active management rather than surgery.
- Trusts can integrate pharmacy into community care
- Avoid medication inaccuracies with new technology
- How to implement medicines optimisation
Motivational factors
What would improve patient adherence?
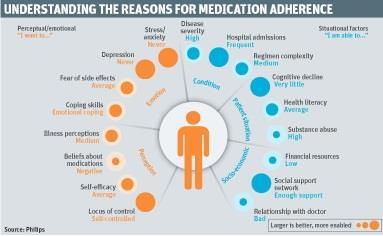
One aspect is understanding what patients are doing and why, and intervening to help them choose the right course (see diagram, below).
King’s Fund fellow in health policy Helen Gilburt says understanding how involved patients are in their health can help predict whether they will stick to medication and also what use they may make of the NHS.
Some patients will have high “patient activation levels” and will see themselves as having a level of control over their own health. Others have a low level and may not feel their actions influence their health. They may not see that medication regime compliance or making lifestyle changes is likely to affect their health.
‘Not understanding a patient’s reasons for not taking tablets can mean the “wrong” solution is offered’
“It is a mixture of health literacy, confidence and people understanding their role and how they can actually make a difference,” Ms Gilburt says. Offering tailored support to patients, according to where they are on this spectrum, can help.
Take patients on medication, for example. Around £300m of medication prescribed in primary care is “wasted”; about half of this is avoidable. Patients may miss doses or give up medication completely for a whole range of reasons. Some of these will be practical but some will be perceptual - they may fear side effects, for example.
Unravelling the reasons for non-adherence could help doctors and others address them effectively. Mr Redding says giving patients the chance to “surface” any concerns is important. But in primary care time can be an issue, especially if patients feel they can only raise one issue a visit.
Not understanding a patient’s reasons for not taking the tablets can mean the “wrong” solution is offered - there is a little point in giving a pill dispenser to someone who is not taking medication for fear of side effects. Yet doctors are often too pressed for time to find out the real reason.
Identifying the issues
Philips has been developing a software based solution to this, which will help health professionals and patients identify and address the reasons behind non-adherence.
“It’s a tool that can bring to the surface the underlying reasons,” says Aart van Halteren, principal scientist at Philips.
“One of the key things in this research is to ask questions of people in such a way that we get a complete view of what drives them.”
‘Ask questions of people in such a way that we get a complete view of what drives them’
This sort of personalised approach can be used in other areas of healthcare. Starting treatment for cancer is a point at which personal preferences can be taken into account with the aim of encouraging patients to play a more active role in their treatment, leading to better outcomes and improved quality of care.
Philips is developing a web based tool that can help achieve this.
But technology can also be helpful in giving people a nudge in the direction of a healthy lifestyle. While many doctors and nurses will try to encourage patients to lose weight and exercise more, this can be difficult to follow up without adding to existing pressures.
Yet patients may start with good intentions and slip back into old habits between appointments. That is where technology can play a part.
Personalised feedback
Keen sportspeople already use activity monitors but they could also be used by the general population and look at indicators such as movement and heart rate. Providing personalised feedback to the patient is an important part of it.
‘This sort of technology can give you continuous support without putting a burden on clinicians’
“With this sort of technology you can have continuous support without putting a burden on the clinicians,” says Mr van Halteren.
Philips has developed an unobtrusive sensor that can be incorporated into a watch, for example. It uses light to measure changes in blood volume and other relevant health parameters, such as heart rate.
This technology has already been incorporated into products aimed at sportspeople but is now being further developed with the aim of being used in preventative healthcare, early diagnostics and eventually continuous monitoring of those who are chronically ill.
Engage and encourage
The sort of simple healthcare procedures that people carry out for themselves can also be made more effective. For example, poor oral health has been linked to serious diseases, including poor cardiovascular health, diabetes and dementia. While most people will brush - and hopefully floss - a harmful biofilm may still build up on their teeth between visits to the hygienist.
Encouraging them to use a toothbrush that uses pressurised air and water to reduce that build-up and reduce inflammation may be one way of getting them to improve their dental health.
‘If you understand the profile of the patient you are in a better position to help them’
“Some solutions will work for one patient but not for another,” says Mr van Halteren.
“Some are really motivated by having group meetings with those who face some of the same dilemmas, some are motivated by seeing the numbers, while others like to see someone in authority - such as a doctor or a coach - who tells them what the next steps should be.
“If you understand the profile of the patient then you are in a better position to help them. It is not just understanding what disease the patient has but what patient the disease has.”
Aart van Halteren on treatment adherence tools
With the average life expectancy predicted to rise to 83 for men and 87 for women by 2032, many of us can look forward to a long and, hopefully, healthy phase of life as we approach our retirement years.
However, while we would hope to maintain good health for as long as possible, some of us will inevitably develop some form of long term condition. How effectively it will be managed will be key to our quality of life and ability to stave off potential medical interventions and hospital admissions in the future.

From the perspective of the healthcare sector as a whole, long term conditions account for 70 per cent of current NHS spending. In light of the UK’s quality, innovation, productivity and prevention drive, greater patient engagement and improved medication adherence will also be critical.
Understanding not just what is the matter with the patient but also what matters to them in terms of personal motivation, knowledge and skills will be central to the level of patient engagement, even before treatment begins.
Here, web based tools such as the Philips Prostaid portal will become increasingly important in enabling shared decision making. Using interactive questionnaires, the patient - together with the clinician - can evaluate and assess the different therapy options in relation to the patient’s personal preferences and quality of life expectations.
‘Patient engagement and improved medication adherence will be critical’
There is also ample opportunity to help stem cost inefficiencies, in particular in the area of medication adherence. Studies show that, on average, 50 per cent of patients with one or more chronic conditions struggle to stick to their prescribed medication regime.
Why, then, is it such a problem? Again, the answer lies largely in having a true understanding of the patient, their abilities and their concerns when they first embark on their recommended course of treatment.
At Philips we believe this patient centric approach is the starting point in collaboration with healthcare professionals, the patient and their family.
Having insights into the barriers and enablers that can impact on the level of adherence will help tailor support to address the patient’s specific situation and needs.
This may take the form of education and coaching sessions, or could constitute practical help for medication intake - all of which are aimed at enhancing motivation, self-confidence, knowledge and skills.
One thing is clear, while advances in medical treatments and healthcare technology continue, they will not be capable of reaching their full potential to reduce the burden of chronic illness if we fail to address and improve patient engagement and specifically, medication adherence.
Aart van Halteren is principal scientist at Philips


























1 Readers' comment