Sid Singh and Alex Barclay discuss the critical challenges at hand, and show how a rapid approach to innovation involving a multidisciplinary team can lead to high-quality solutions
![]()
This is paid-for content from our commercial partners. Find out more
As the world continues to tackle covid-19, the NHS is facing an elective care backlog in excess of 5 million patients. All of these patients are suffering extended waiting times for important surgery. The pandemic has fuelled this challenge as healthcare professionals (HCPs) worked tirelessly to treat victims of the virus. Linked to this is a second challenge: record level burnout in staff. The result is patient disempowerment, which in turn leads to further exacerbation of issues relating to the backlog and HCP burnout rates. An ongoing vicious circle.
This challenge is not exclusive to the UK. Covid-19 challenges are creating massive pressure to health services globally. In the case of HCP burnout, 50 per cent of medical staff in the USA[1] were found to have been impacted, as medical staff try to respond to their own backlog.
Recognising the urgency of this, we assembled a diverse team of experts with the goal of using design thinking to identify innovative human-first healthcare solutions. Made up of clinicians, technologists, business strategists, software engineers and data scientists from the NHS, Harvard Medical School, the Boston Consulting Group and the Royal College of Art, and powered by innovation ‘do tank’ Fuzzy.org, the team collaborated virtually to rapidly develop and test a set of concepts. This agile, human-centred design approach enabled us to achieve high-quality outcomes in days not weeks.
Approach
Our aim was to create a set of resources that can be used to help tackle the elective care backlog, empower patients to get the treatment outcomes they need, and prevent HCP burnout.
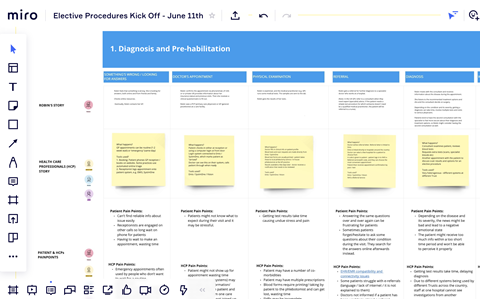
Using MIRO, our first step was building an elective procedures ‘blueprint’ – a map of the clinical pathway with pain and gain points captured. We did this via ‘virtual Gemba walks’ where one-to-one interviews with patients and medical staff helped the team capture deep insights about human and technological needs.
Next, the team generated ideas and stress-tested them with other healthcare professionals and patients. Once the ideas had been validated, we identified the realistic next steps required.
10 experts, 8 hours, 12 tested ideas
Through multidisciplinary, expert collaboration and human-centred design, the team achieved what would traditionally take multiple weeks in just eight hours. The concepts developed explore ways of leveraging technology in a human-first way to improve the experience of everyone involved in clinical pathways, at scale. Many ideas benefit both clinicians and patients, and at various different points in the patient journey. Below is a sample snapshot of two ideas generated. For the full set and more on how we worked, see our peer reviewed whitepaper here.
Our Rapid AI Prioritisation and Routing concept (Idea 2) demonstrates the beneficial application of artificial intelligence. The clinicians we worked with identified a key pain point associated with the accurate prioritisation of patients. The current inability to do so is a key contributory factor in the growing care backlog, with staff finding it difficult to precisely identify, prepare and route patients for surgery.
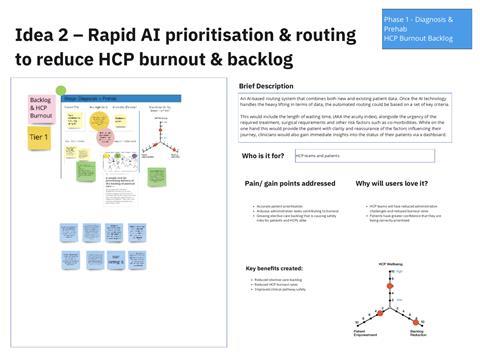
To solve this, the team considered ways in which AI could handle the heavy lifting when it comes to data, before automating the routing process based on a set of key criteria. Criteria include the length of waiting time (AKA the acuity index), co-morbidities and other risk factors, alongside the urgency of the required treatment and surgical requirements. With automated routing, HCP teams experience a reduction in administrative strain, while patients receive the right treatment in a timely manner. As an extension of this idea, HCPs could be equipped with a dashboard to gain immediate patient status insights.
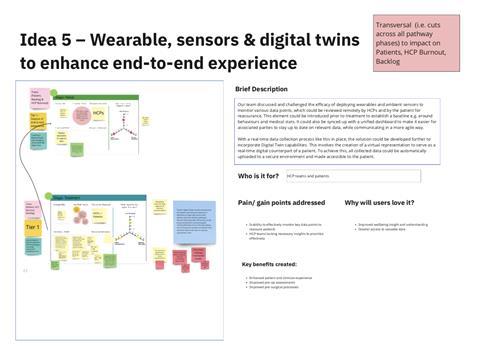
In Idea 5, the team explored the benefits of deploying wearable monitors, ambient sensors and Digital Twin technology for patient recovery. Devices capture various data points in real-time prior to and post operation which are viewed by clinicians and patients. Incorporating Digital Twin technology enables the creation of a digital counterpart of the patient, providing a virtual representation for HCPs to monitor and analyse. The technology is leveraged to ensure that patients and clinicians capture and see data and progress made in a no-effort way.
Clinicians critiquing this idea thought it would be extremely useful for minimising on-the-day delays caused by patient absence or unreadiness. It would also help speed up the discharge and at home rehab process. Overall benefits include reducing the elective care backlog, empowering previously frustrated patients, and helping prevent burnout by reducing the administrative burden.
Raising awareness
Our aim is to show healthcare decision-makers the approach and the ideas so they can be taken forward, be built on and scaled as needed. For more details download our whitepaper here.
Sid Singh is chief clinical informatics officer and chief medical information officer, George Eliot Hospital Trust
Alex Barclay, is the founder of non-profit innovation ‘do tank’ Fuzzy and strategic design principal, Boston Consulting Group
Source Date
[1]Trends and Factors Associated with Physician Burnout – pp. 2

























