Virtual ward for patients undergoing total hip or knee arthroplasty can turn the tables around for postoperative capacity and help downsize the waiting backlog

Waiting too long for joint replacement surgery can have lifelong consequences. It can lead to loss of independence and confidence, increases the risk of falls and emergency surgery, and can contribute to a more difficult recovery and poorer outcomes. A recent study found that patients (n=326) waiting over six months for a total hip or knee arthroplasty experienced a significant deterioration in their health-related quality of life and increased frailty (Clement et al, 2022).
Sponsored by
In August, over 700,000 people in England were waiting for specialist orthopaedic treatment, with patients waiting 29 weeks on average. Postoperative capacity presents a critical challenge for addressing this backlog and can limit the number of operations that are able to be performed.
Potential solution
In September Doccla and its NHS partners launched its first postoperative virtual ward for patients undergoing total hip or knee arthroplasty.
The aim of the virtual ward is to enable safe early supported discharge to:
- Support patients to better manage their recovery following discharge;
- Allow patients to recover from their operation safely and conveniently at home; and
- Free up bed capacity so that more patients can get their joint replacement surgery sooner.
What does Doccla do?
Doccla provides a wrap-around virtual ward service. It includes the monitoring equipment, software (including the patient app and clinical dashboard), logistics (including delivery and collection of the equipment) and a dedicated patient and clinician helpline from 8am to 9pm.
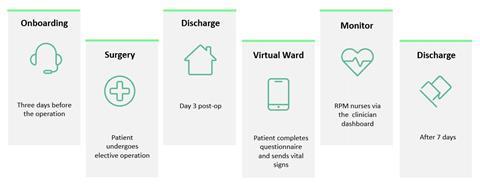
How does the virtual ward work?
Patients receive an “onboarding call” and a Doccla Box containing all the monitoring equipment three days before their operation. The Doccla Box contains:
- A pre-configured smartphone with the Doccla patient app;
- Blood pressure monitor;
- Thermometer;
- Pulse oximeter;
- Patient information sheet; and
- Haemoglobin and blood glucose monitors (if required).
Patients start using the equipment on arrival home, usually on day two or three after their operation. They record their vital signs using the equipment and complete a questionnaire about how they feel using the patient app. Patients can also take and send photos of their surgical wound through the app and receive video calls for their clinicians.
Remote monitoring nurses can then view each patient’s vital signs and completed questionnaires on Doccla’s clinician dashboard. They decide how often patients need to enter their readings and decide when they can be discharged.
Doccla’s customer service team also monitors the dashboard and contacts patients who have not entered their measurements. This allows the team to assist patients who are having difficulty using the equipment and ensures that clinicians have access to accurate, up-to-date information.
Outcomes
The first 10 patients have been admitted to the postoperative virtual ward. So far, patient compliance has been high, with 100 per cent of patients submitting their information at the agreed times and none of the patients have required readmission.
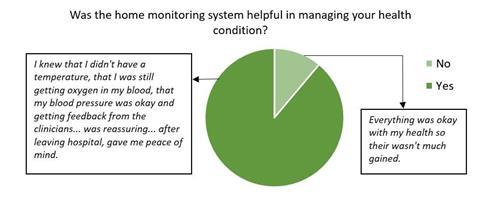
Nine patients have provided their feedback so far. Importantly, 89 per cent of patients (n=8) reported that the service helped them to manage their health after they were discharged. The majority of patients also reported being “satisfied” or “very satisfied” with the service (n=7).
One patient described their experience during a Sky News interview. They said: “My wife is infirm. Although she’s got carers, I’m her main carer. So I have to look after her…So I wanted to be at home with my wife.”
Giving feedback to the team, he added: “Really nice to know that I was being taken care of from my own home.”
The Academic Health Science Network is currently evaluating the impact of the service on patients’ length of stay in hospital. However, preliminary data based on admission and discharge dates indicates that the average hospital stay for patients using the virtual ward has been shorter than the national average for total hip or knee arthroplasty.
Next steps
Feedback from patients highlights that clear information about what to expect from the service, given at the right time, is essential to a positive patient experience. This feedback, alongside findings from the AHSN evaluation will inform improvements to the service.
As the service grows, Doccla and their NHS partners will continue to safely free up capacity, and in turn promote good patient outcomes and the best possible patient experience.
References
Nick D. Clement, Neil R. Wickramasinghe, John M. Bayram, Katie Hughes, Erlend Oag, Nicholas Heinz, Ewen Fraser, James G. Jefferies, Graham F. Dall, Andy Ballantyne, and Paul J. Jenkins (2022) Significant deterioration in quality of life and increased frailty in patients waiting more than six months for total hip or knee arthroplasty. The Bone & Joint Journal 104-B (11) https://doi.org/10.1302/0301-620X.104B11.BJJ-2022-0470.R2




























No comments yet