Virtual wards are a new, innovative operating model for healthcare, designed to help safely manage healthcare needs at home. With a smart, integrated approach that combines face-to-face contact with virtual environments, virtual wards can be the next leap forward for connected, efficient healthcare.
An ageing population, cost limitations and a large patient backlog have meant a large number of patients occupying beds unnecessarily, with few alternative options for managing their care. IT transformation and the opportunity to digitalise certain elements of interactive care, could offer a route to reducing the strain on doctors, patients and operations.
Sponsored by
With 7.8 million patients on the NHS waiting list as of September 2023, virtual wards enable valuable hospital beds to be freed up for critical care, significantly improve the patient experience and drive better patient outcomes.
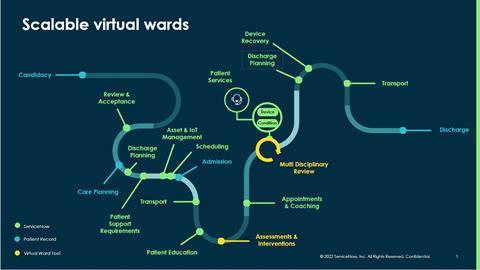
Virtual wards help clinicians to manage patient care and ongoing treatment remotely, allowing patients to remain at home, reducing capacity issues and ultimately improving patient outcomes. Virtual wards can enable remote monitoring, communication, and management of healthcare, in combination with regular face-to-face contact. This is a practical, pragmatic approach, that can broaden access to quality healthcare and give patients the care they need, where they want it.
A scalable solution
Virtual wards require sophisticated measurement and communication technologies to be integrated in real time at the point of delivery. With a combination of new infrastructure, monitoring technology, continuous two-way engagement and regular face-to-face touchpoints, virtual wards transform how technology is applied to healthcare, driving better experiences and increasing agility.
Building blocks of success
For virtual wards to work, hospitals require the right blend of technology and data to connect patient experiences with clinical expertise. From IoT-enabled diagnostic equipment to walking frames and bed pans, there is a lot of simple yet essential equipment required.
Acute hospitals must have a clear, up to date view of their inventory and which patients are using them in their homes. Visibility is also crucial for monitoring repairs or replacements.
Two-way communication is key, with the ability to automatically direct patient enquiries to the right person, analysing and prioritising in real time to give patients the ability to self-serve and accelerate resolutions.
Efficiency will rely on optimising the scheduling and orchestration of visits, with a succinct view of the right information that adapts to the patient’s situation drawn from multiple systems. It’s imperative to implement a reliable, scalable digital foundation which can reduce the complexity of patient journeys to coordinate care across virtual and real-life environments.
Building a solution
ServiceNow is already partnered with the NHS to drive better experiences and efficiency through digital transformation. Virtual wards are the next step forward as we seek to create a streamlined NHS, with reduced pressure on staff and patients alike.
Discover how ServiceNow is supporting the NHS to deliver patient services with more agility and connections here.

























