Daan Dohmen explores why greater integration of virtual wards is needed and the benefits that improved education and guidance for patients throughout their entire journey can bring
An article about the costs of virtual wards published in HSJ in January, created quite a stir. And rightly so. If a 40-bed virtual ward indeed costs nearly twice as much as traditional inpatient care, is this development really in the right direction?
Sponsored by
The discussions that followed mainly focused on the methodology of the study. However, I believe the core issue should be about something else. Based on my experience as a professor of digital transformation in healthcare and as the founder of Luscii, which has implemented more than 350 remote monitoring pathways in 11 countries, here is my opinion on what’s missing and what we can do about it.
How did virtual wards originate?
First, it’s important to look at the emergence of virtual wards, especially their rapid acceleration in England. During the pandemic, the biggest bottleneck in many countries was the availability of acute inpatient capacity. By starting with virtual wards, patients could go home sooner and be monitored at home on various vital parameters, so immediate bed space was freed up. England was one of the most successful countries in Europe in scaling up this concept quickly and realised, after the pandemic eased, that this was beneficial for many conditions beyond covid. Thus, virtual wards proliferated, and significant budgets were allocated to them.
Tip of the iceberg
I often speak with great enthusiasm on international stages about how the NHS has made this movement so quickly and successfully. I am very proud that we are involved throughout the UK in beautiful examples of this innovation, such as in Wolverhampton, Sunderland and South Tyneside, and Maidstone and Tunbridge Wells, to name a few. But I also explain that virtual wards are just the tip of the iceberg for two reasons:
- They often focus on hospital discharge. Although this is an important factor, preventing admissions makes the real difference in terms of health economy costs and outcomes
- They are mainly concerned with vital signs monitoring. Again, vital signs are crucial for managing long-term conditions, but education and self-care have a much greater impact over the medium and long-term.
From early discharge to preventing admissions
First, virtual wards primarily guide patients at home so they can be discharged from the hospital. There is a step up approach in more and more virtual wards, however, the duration of guidance is often relatively short, effectively meant as a replacement of a hospital bed. Yet, patients’ recovery often takes much longer. This is especially true for patients with a chronic condition, such as those with heart failure or chronic obstructive pulmonary disease who are frequently admitted with exacerbations. Their condition generally worsens over time, so after discharge from the hospital or virtual ward, it’s a matter of waiting for another admission to occur.
Essentially, virtual wards are very useful for hospital outflow, but if we do nothing about the inflow, it’s like mopping with the tap still running.
Helping patients to help themselves
The second point concerns the current funding of virtual wards in England, which mainly focuses on equipment that can measure vital signs. Of course, this is useful from an early discharge perspective, but if you also want patients to recover in the long term and prevent admissions, you need to focus on education and self-care in addition to monitoring. This enables patients (and their carers) to take ownership of their healthcare journey and ultimately help themselves, reducing in-person visits.
Combine this with timely detection of deterioration and we will really start to see reduction of pressure on the entire system, not just the wards, but also primary care, community care, and accident and emergency.
Digital care, like in other countries, should also be viewed in an integrated manner in the NHS
800 per cent ROI possible
Is this a utopia? Not at all. In many other countries, virtual wards are part of an integrated approach primarily aimed at saving healthcare providers’ time by preventing unnecessary care. For example, the academic hospital in the city of Utrecht in the Netherlands realised a return on investment of 800 per cent in the Safe@home program, where patients are proactively guided to prevent unnecessary care, including admissions and hospital visits.
Of course patients can conduct measurements of vital signs with connected devices (such as blood pressure or heart rate) in our Luscii app, but crucially, this is combined with fully automated self-care and educational content in a guided timeline, so that the patient also learns to notice and take action to prevent deterioration.
Similar projects are seen in Ireland, where our platform is used nationally in primary care by general practitioners for heart failure and COPD. In Germany, a pathway for patients with severe lung conditions was recently launched at the prestigious University Hospital in Essen. And in Africa, patients with hypertension and diabetes are equally managed successfully this way.
UK examples: Reduction in admissions, A&E and primary care usage
Luscii is delivering similarly impressive, well researched results in the NHS. Despite funding that is mainly focused on virtual wards, we have worked with some teams to enable an approach that can provide support along the whole pathways of care.
For instance, Imperial College in London managed to reduce their A&E attendances by 65 per cent and their unplanned admissions by 81 per cent with this integrated approach of remote monitoring, education, and self-care. As such, they also made savings of £398,000 in the first 90 days after implementation.
Similar figures are seen in Sunderland, where the ROI was 625 per cent while the number of respiratory emergency admissions decreased by 58 per cent and primary care usage by 34 per cent.
As impressive is the Digital Care Hub in Airedale, which now guides one of the NHS’ largest COPD cohorts, managing thousands of patients in this integrated way, or as they call it, “remote monitoring and supported self-management for people with COPD”. The results are equally positive. So far, Airedale has seen a 50 per cent reduction in non-elective admissions and a 21 per cent reduction in A&E admissions.
A system wide platform for (health) care at home
I definitely think the authors of the study which HSJ reported on make an important point and actually expose what the next steps should be. Digital care, like in other countries, should also be viewed in an integrated manner in the NHS. Of course, activities need to focus to enable early discharge, but this is only part of the puzzle. Patients also need to be provided with education and guidance throughout their entire journey so they can learn to help themselves and avoid admissions. Otherwise, it’s like building a hospital without a clinic or general practice nearby. Digital care, just like regular care, is integral and requires us to view it as such.
Connecting the dots: a pyramid model
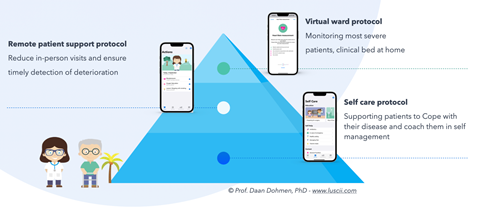
I call this method “connecting the dots”, based on our pyramid model whereby the Luscii App (automatically) adapts to different situations. At the top, are virtual wards focusing on monitoring vital signs. The layer below is “remote monitoring and supported self-management” and, besides monitoring, is mainly about education and guiding patients remotely so that admissions and readmissions are prevented. In the bottom layer, patients are guided to live independently with their condition and detect deterioration. This supports general practitioners, community care, acute and A&E.
Just as patients go through this pyramid (from top to bottom and vice versa), so should the funding and technology. Then a system-wide platform for (health) care at home emerges. Then we really support, not just the patient, but also the healthcare providers in acute, community, and primary care.
Let’s share our knowledge to create our future.
We would love to show you what we can do either in the UK or in one of the other 10 countries where we are active. Hopefully by sharing what we do, we can create our own future together.
To learn more about Luscii’s digital remote monitoring solutions, visit our website.



























