AI holds the promise of being a major boon to the NHS. But so far, we have not seen AI have the impact that it has promised. The big challenge is making the leap from one-off pilots and innovations to systematic use across the NHS. In this article, BCG outlines five steps that the NHS – at national and system level – can take to move from pilots to impact at scale.
Sponsored and written by
The NHS is at a critical crossroads. Demand is outpacing supply, budgets are stretched, and workforce shortages continue to strain the system. Without bold changes, projections suggest an extra £90bn[1] of funding will be needed over the next decade to meet demand. Artificial intelligence offers one way forward – not just as a means of easing the pressures of today – and tomorrow – but to position the UK as a global leader in AI-driven healthcare.
AI in healthcare also has the potential to generate significant revenue: the UK has established a flourishing digital health sector, with more than 3,000 UK-based AI companies generating more than £10bn revenue in 2023[2], and UK health tech startups raising $2.3bn in 2024.[3]
Health and social care secretary Wes Streeting has made his position clear: the NHS must shift from “analogue to digital”. AI will be central to this transformation. The good news? AI is already showing its potential. On the clinical side, machine-learning-based lung cancer detection tools like Behold.ai are helping speed up diagnoses, while other ML-based models such as the Cambridge-developed C2-AI can predict NHS hospital admissions before they happen. From an administrative perspective, AI tools could be similarly transformative, with Microsoft’s ambient listening technology, DAX copilot, able to automatically transcribe notes from patient-clinician interactions and drop them straight into a patient’s record.
But despite the excitement, adoption remains slow. Why? The UK faces particularly high barriers – low public trust, fragmented policies, and regulatory bottlenecks – that are keeping AI from scaling across the NHS.
What’s holding AI back in the NHS?
A recent white paper co-published by the World Economic Forum and Boston Consulting Group[4] confirms that AI adoption is not just a UK problem, it is a global challenge. However, it seems that the UK is particularly affected by barriers to adoption. To name a few:
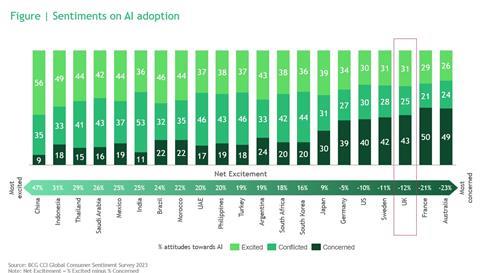
Trust building: NHS staff are broadly positive about the potential of AI in healthcare, with more than half of doctors saying they are “optimistic” about it in a recent survey. Yet nearly 70 per cent of them said they had not received adequate training to understand their responsibilities when using these systems.[5] Additionally, compared to most countries in the world, the UK public is among the most concerned about AI adoption, making confidence-building crucial.
Lack of coherent implementation of the national AI strategy: fragmented policies, short-term funding cycles, and interoperability issues create a “stop and start cycle”, making it hard to maintain momentum.
Slow and conservative regulatory processes: AI evolves fast, making it difficult for regulators to keep up. This means approvals are currently a lengthy and uncertain process.
So, what would the future look like if we overcame these challenges?
AI at scale in the NHS isn’t just a distant dream, it is within reach. Imagine a world where AI-powered tools help doctors predict patient deterioration before it happens, automate admin tasks to free up staff time, and optimise hospital resources to cut waiting lists.
With its unparalleled multi-modal dataset, the UK could be a global leader with a robust pipeline of AI solutions, co-developed with industry and tailored to real NHS challenges. Local pilots would be the testing ground, allowing rapid deployment and real-world learning before a national rollout. Scaling up would be rapid and systematic, with only the best, most evidence-backed AI tools adopted widely.
The time and cost savings AI brings could be reinvested into patient care, supporting more frontline staff and better services. AI wouldn’t just be an add-on; it would be at the heart of a more efficient, proactive, and patient-centred NHS.
We outline five key steps to make this vision a reality.
To move AI from pilot mode to real-world impact, action is needed at every level:
- National leadership (NHS England and the Department of Health and Social Care) must set the right conditions for AI adoption
- Local providers and systems must identify the highest impact areas and integrate AI into daily operations
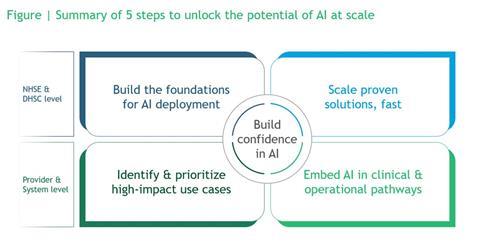
Here’s how both levels can play their part:
1. Build the foundations for AI deployment (NHSE and DHSC level)
Too often, AI initiatives fail on the barren soil of healthcare systems ill-equipped to take advantage of the promise. AI requires system-level readiness – of its staff and its systems – to ensure proper adoption:
- Train NHS staff on AI literacy
- Standardise toolkits and playbooks to support smooth integration
- Create ‘deployment networks’ to scale successful pilots across regions and shape and support an ecosystem of AI players
2. Scale proven solutions – fast (NHSE and DHSC level)
It seems that every month, news of a groundbreaking AI pilot reaches the news. But too often, these AI projects stall after successful trials. Scaling initiatives requires a set of capabilities that can be hard to find in the NHS. To fix this:
- Set up national innovation zones, with hub-and-spoke or “fast follower” models to spread AI solutions efficiently
- Build strategic partnerships with private sector leaders on AI
- Shift to a risk-based, adaptive regulatory framework
3. Identify and prioritise high-impact AI use cases (Provider and System level)
Implementing and scaling operational AI should come first to prove early value and focus resources. The NHS has traditionally favoured a more “thousand flowers blooming” approach – emphasising local innovation and independence. We argue that in a resource-constrained environment, the NHS should focus on maximising value by prioritising AI where it can make the biggest difference:
- Be clear on the high-volume, high-cost areas such as cancer screening (MIRAI) and primary care decision support
- Use rapid trials and systematic reviews to assess cost-effectiveness and real-world impact
- Build centralised evaluation frameworks – utilising the hubs to assess each other, and streamline AI approval and regulatory processes
4. Embed AI into clinical and operational pathways (Provider and System level)
For AI to have a lasting impact, it cannot remain an add-on to existing pathways. Instead, more must be done to ensure that AI solutions become a seamless part of NHS workflows:
- Integrate AI into clinical pathways and governance frameworks
- Implement robust post-deployment monitoring to track safety and effectiveness
- Establish stable reimbursement mechanisms to sustain AI-driven innovation
5. Build confidence in AI (Across all levels)
Ultimately, it is patients and staff that will determine the success or failure of AI, by choosing whether to adopt the new technology. Public and NHS staff trust is crucial for AI’s spread in the NHS – and so the NHS should take a proactive approach to building trust:
- Ensure transparency and explain how AI support, not replace, clinicians
- Showcase real-world impact and safety, such as faster cancer diagnoses and reduced wait times
- Engage patients in AI through advocacy groups and user-friendly tools
- Leverage Royal Colleges and NHS leaders to champion AI through public awareness campaigns
Why this matters now
Momentum is building – AI breast screening trials are expanding, and NHS leaders are optimistic about ambient listening technology. But progress is too slow. And, with staff overstretched and patients waiting to be treated, the NHS cannot afford to wait any longer.
By acting at both national and local levels, the NHS can move from AI pilots to full-scale deployment – quickly, safely, and effectively.
Special thanks to Anna Nedey for her support with this article
Source
[1] Rocks et al. (2024) ‘How much funding does the NHS need over the next decade?’. The Health Foundation
[2] Clark, F. (2024). Artificial Intelligence sector study 2023. Department for Science, Innovation & Technology
[3] Adams, L. (Oct 2024). Health tech and life sciences lead the way for UK VC investment in Q3
[4] World Economic Forum (co-developed with BCG) (2025). The future of AI-enabled health 2025
[5] Alan Turing Institute (2023) ‘Majority of doctors using AI are optimistic about its benefits’. Alan Turing Institute News
[6] World Economic Forum (co-developed with BCG) (2025). The future of AI-enabled health 2025

University hospitals key to unlocking UK’s £78bn healthcare innovation potential
Unlocking the power of end-to-end digital solutions in healthcare: Global insights for the NHS
Climbing blind up the productivity mountain: how transparency, equity and trust could deliver care for 10-15 million more patients



































2 Readers' comments