Salford Royal Foundation Trust is taking steps to apply the main themes of the Francis report. Namely recognising warning signs and promoting openness, leadership, transparency and candour. Jenna Tsai, Chris Brookes and colleagues explain
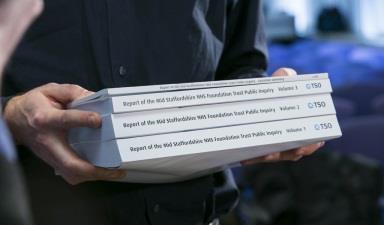
Recommendation 1 of Robert Francis’ Mid Staffordshire public inquiry report includes a call to action for all organisations working within healthcare to consider his report and decide how to apply its findings.
Although Salford Royal Foundation Trust had already made inroads into understanding how the Francis report might apply to the organisation, training was sought to better understand its key themes. Hill Dickinson’s training covers warning signs at Mid Staffs (and how organisations should deal with them), openness, leadership, transparency and candour.
‘“What matters most to you?” whiteboards are already in use on some wards to prompt clinicians to treat the person before the condition’
Salford Royal has statistically better than expected risk-adjusted mortality, a proven track record of reducing harm to patients and an ambitious plan to put its patients at the heart of everything it does. However, even “good” trusts can learn from the Francis report.
The trust commissioned a team of leaders from within the trust to review the report’s recommendations and to assess its position. Early conversations already point towards a redesign of trust strategy.
Listening to patients
Real patient empowerment requires a paradigm shift in the traditional doctor-patient hierarchy, as well as challenges to stereotypes of patients. The trust identified barriers to empowering patients further and clinicians were conscious of the potential impact on their time.
‘There have been numerous examples of successful changes that were solely developed by frontline staff’
It is considering introducing patients as coaches, including them in service reviews and ward rounds. It proposes to collate patient experience data by consultant level and to prompt clinicians to ask patients in clinics “What matters most to you?” This is to ensure that, as well as the provision of safe and clinically effective care, the patient feels that their particular concerns have been addressed.
Whiteboards asking “What matters most to you?” are already in use on some wards to prompt clinicians to treat the person before the condition. Patients, particularly those with long-term conditions, are often self-taught experts in their individual complaint and their expertise and autonomy should be respected in determining their clinical plan.
Listening to staff
The chosen improvement methodologies – the Model for Improvement and the Breakthrough Series Collaborative – are based around empowering frontline staff to use their expertise to solve problems.
There have been numerous examples of successful changes that were solely developed by frontline staff. However, those staff do not always hear consistent messages from managers and there is a recognition that more could be done to empower them.
‘The North Shore Long Island Jewish Health System ses weather forecasts to predict A&E usage – this is the kind of smart use of data we wish to implement’
During a transfer to become “paperless”, wards at the trust were told that stool charts would be added to the electronic patient record system. Some wards objected as these charts were used collaboratively with the patient, which would no longer be possible once the chart was digitised. These objections were not listened to because the trust objective was to “go paperless”.
Why didn’t managers take notice as to why clinicians objected to the change? Why didn’t the clinicians feel empowered enough to push back? The ideal situation would have been one where both managers and clinicians with the same goal – patient safety and quality care – sat down to devise the best outcome, balancing the positives and negatives for each solution.
The team is recommending that focus on culture be a “big dot” aim in the next strategy, with numerous culture-specific interventions including:
- implementing a safety culture survey;
- teaching human factors and situational awareness; and
- HR practices to support a culture of safety including shifting job plans.
Warning signs
The Francis report includes a chapter dedicated to the warning signs that were present at Mid Staffordshire. Current measures of performance are based on past performance. Measurement methods are largely based on national priorities and tend to focus on indicators that are simpler to measure, rather than clinician recognition of harm.
The trust’s vision is to move to an information system that considers both the present and the future. It would like its systems to be able to alert clinicians when harm is about to happen and to hold greater real-time information. The North Shore Long Island Jewish Health System, in New York City, uses weather forecasts to predict A&E usage – this is the kind of smart use of data we wish to implement.
Can we predict harm before it happens and react based on data? While past performance is important, the ability to predict future performance is a huge step to achieving unprecedented levels of safety.
To the future
In designating a team to review the Francis recommendations, it became clear that a wholesale redesign of Salford Royal’s quality strategy was needed. Improvements based on the recommendations could be made sporadically but the trust is looking past mere improvement towards radical redesign, with the aim of becoming the safest organisation in the country. Several primary drivers of the new strategy have been proposed including:
- a step-change in doctor involvement in quality and safety (job plans, rewards, consultant level data, shadow coaching);
- first-class support services (including HR, data support, communication, etc);
- a shift from retrospective data to real-time and prospective data;
- a step-change in listening to patients – how can we move past surveys?;
- a step-change in listening to staff – how do we react to cues from the frontline swiftly?;
- a focus on flow and demand/capacity management;
- developing effective local learning systems.
In order to complete this process, the trust will take time to engage with patients and staff at all levels to be sure the final strategy fits the needs of all.
Jenna Tsai is a solicitor at Hill Dickinson. Chris Brookes is executive medical director; Elaine Inglesby-Burke is executive nurse director at and Siobhan Moran is assistant director of quality improvement at Salford Royal Foundation Trust























No comments yet