Welcome to the interim report of HSJ and Serco’s Inquiry into Maximising the Contribution of Non-Clinical NHS Staff, which is examining how to get the most from this key part of the workforce – and how to give the most back to them in terms of rewarding careers
Over recent years, a remarkable consensus has formed in NHS policy that the service’s future must be one of planning and providing person-centred care services on a health and care economy-wide basis, delivered by clinically led multidisciplinary teams working together with patients beyond traditional organisational silos.
These themes inform and illuminate the Five-Year Forward View strategy, and all subsequent major policy initiatives.
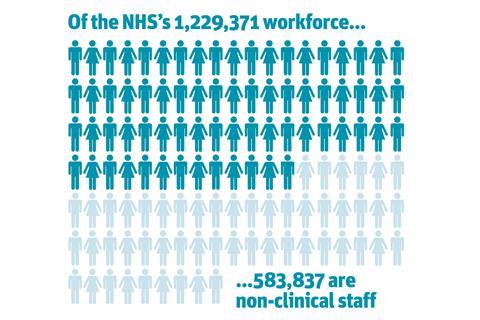
It all sounds attractive. Yet although this narrative has developed alongside an aspiration to get clinicians involved in changing care planning and provision, it has tended to include very little or nothing about the contribution and value of the 583,837 non-clinical members of the NHS’s 1,229,371 staff.
The very term “non-clinical” may be part of the problem. Defining any group negatively, as what it is not, is scarcely the best way to think about that group.
The term also suggests that for all the rhetoric about teamworking, there remains a gap and hierearchy between clinical and non-clinical staff every bit as polarising and unhelpful as those between and within the clinical and medical professions (which would be another inquiry altogether).
One very positive outcome of this inquiry would be to find a better descriptive term for these staff than “non-clinical”: we welcome your suggestions hsjinquiry@emap.com.
The invisible half of the NHS workforce
The value of clinical staff in the NHS scarcely needs stating (although junior doctors might currently disagree). Contrastingly, non-clinical staff can seem and definitely feel rather invisible in discussions about workforce, training and policy.
This interim report, based on interviews with sector experts and a half-day workshop, aims to focus attention on the contribution and value of these staff, whose sometimes unseen and often under-recognised work make crucial contributions to the running of services.
As the NHS plans radical changes in provision with the Carter efficiency review, the 44 sustainability and transformation plans and footprints, success regimes, devolution in Manchester, its chances of success will need considered, consistent, credible and sincere engagement with all its staff groups.
If we are to see real change in the NHS, it will mean real change in how all the health and care team – clinicians, medics and non-clinical colleagues – work. It will also mean investing in training and change management capacity: particularly (thought not exclusively) among non-clinical staff.
Forward-thinking clinical staff have long valued all the members of the health and care team, including their non-clinical colleagues: it’s time that everyone else did.
- As of September 2015, the NHS total workforce is 1,229,371 hospital and community health service staff.
- 647,907 are ‘professionally clinically qualified’; of this group, 113,750 are doctors (including locums).
- There are 369,939 support to clinical staff and 213,898 NHS infrastructure support.
- These 583, 837 non-clinical staff are the focus of our inquiry
- The total non-medical workforce is 1,115,722. This includes: the 357,099 qualified nursing, midwifery and health visiting staff; the 158,135 qualified scientific, technical and therapeutic staff, and the 19,160 qualified ambulance staff.
- Non-clinical staff breakdown: 213,898 are NHS infrastructure support (63.3 per cent) and 369,939 are support to clinical staff (36.6 per cent)
Source: latest HSCIC data, September 2015
The value of non-clinical staff
This inquiry focuses on non-clinical staff other than those at board level. As such, it will not repeat arguments about the value of managers which HSJ has previously addressed nor address the issue of leadership, again the subject of recent work by HSJ.
Defining any group negatively, as what it is not, is scarcely the best way to think about that group
To exhaustively catalogue the many categories of role under the non-clinical umbrella wouldn’t add huge value. As well as key services provided by cleaners, cooks, porters, gardeners and maintenance colleagues, there are administrators at all levels, switchboard colleagues, IT staff, security staff, as well as those in communications, finance and HR.
There are receptionists, including those in GP practices. And there are the staff who handle arguably the key litmus paper issue of the NHS: car parking. The NHS could not function without these people’s contributions.
How HSJ readers can help
There is relatively little research or study specifically of the NHS’s non-clinical workforce. As such there is not a large body of existing literature on which to draw.
When the launch of this inquiry was announced, we asked HSJ readers for good practice examples and case studies, some of which are available online.
From our research and meetings so far, we developed some ideas which run through this interim publication – and a series of self-assessment questions to help all NHS organisations, as well as system leaders, policy makers and politicians, to reflect on their practices and plans for the non-clinical workforce.
We want to hear your case studies of good practice. We also greatly welcome your feedback and challenges on our interim thoughts and suggestions. Your comments and responses to this publication will help shape the remainder of our work and the final report, which will be published at the HSJ Summit in November.
We look forward to hearing from you: hsjinquiry@emap.com
Downloads
maximising non clinical workforce interim report
PDF, Size 1 mb
Mobilising the NHS’s hidden army
Interim report of HSJ and Serco’s Inquiry into Maximising the Contribution of Non-Clinical NHS Staff
 Currently
reading
Currently
reading
Mobilising the NHS’s hidden army
- 2
- 3
- 4
- 5
- 6
- 7




































5 Readers' comments